It’s no surprise that huge changes are currently happening – and will continue to happen – in the senior care sector as a result of COVID-19. Care homes, extra care facilities, and anywhere there’s retirement communities have been disproportionately affected by the virus.
At the same time, 2020 has seen massive investment in the sector and new care homes being built thick and fast. As a result, more and more care providers are starting to look at future-proofing their properties with COVID and any other potential pandemic or sanitation issue in mind.
There are two sides emerging, creating a new approach to care home design. The first is the practical side – making things physically safer.
For example, in order to allow external visitors, we’re seeing the implementation of isolated visiting rooms in various guises. Some providers have opted for dedicated rooms with a direct external point of access, easy to clean and ensure a well-managed, safer visit. Others have taken this a step further by adding glazed partitions to these externally accessed, dedicated visitor rooms, still allowing residents to see and speak to their loved ones without physically being in the same space. This approach means that these important family interactions can still take place without visitors ever having to step foot in the body of the main home, thereby keeping residents, their visitors and staff safe. The rooms still have comfortable furniture, so both party members are able to sit for an informal visit, with a face-to-face link – but safely.
Within the buildings, care homes are now putting extra consideration into layout and infrastructure. This can involve things like multiple access points – allowing staff, residents, deliveries and visitors to access the building via individual entrances, keeping circulation separated. Corridors are now being designed with one-way systems, including additional cross corridor, fob-controlled doors, allowing zones of the building to be isolated should containment be required, also introducing passing points within corridors and increased floor space around lifts and staircases to accommodate good social distancing.
I’ve also been looking into the installation of water and power points at ambulance stations, to allow for easy mobile testing moving forward.
The second side of the new approach focuses much more heavily on the personal aspect of COVID and how it has directly affected residents’ mental health. One of the most impactful side effects of COVID – aside from the virus itself – has been the immense isolation it has caused in these communities.
It’s just as important to think about mental health as it is physical health – and the segregation and isolation caused over the past 8 months is one of the larger issues to overcome. For good mental health, we all need interaction – whether that be with friends, family, care staff or other visitors.
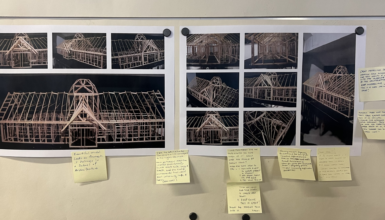
This is one of the problems I have been trying to address in recent presentations with care providers. I’m particularly enthused by the Household Theory. This is a traditionally Dutch approach, whereby residents don’t live in the traditional care home environment with a large communal area. Instead, the residence is split into individual households, typically housing around 10-14 people. Each household has its own kitchen and lounge in a far more residential setting. This reduces risk by reducing external interaction – but allows for interaction among the household ‘bubble’. The number of staff entering each household will be reduced in this scenario, as the staffing ratio reflects the number of people living in each individual household.
Whilst this is not an approach we can easily adapt into existing care homes – it’s certainly worth considering when future-proofing new builds. It addresses both the physical safety and the mental wellbeing of all involved – something which I feel we’ve all seen the importance of this year.